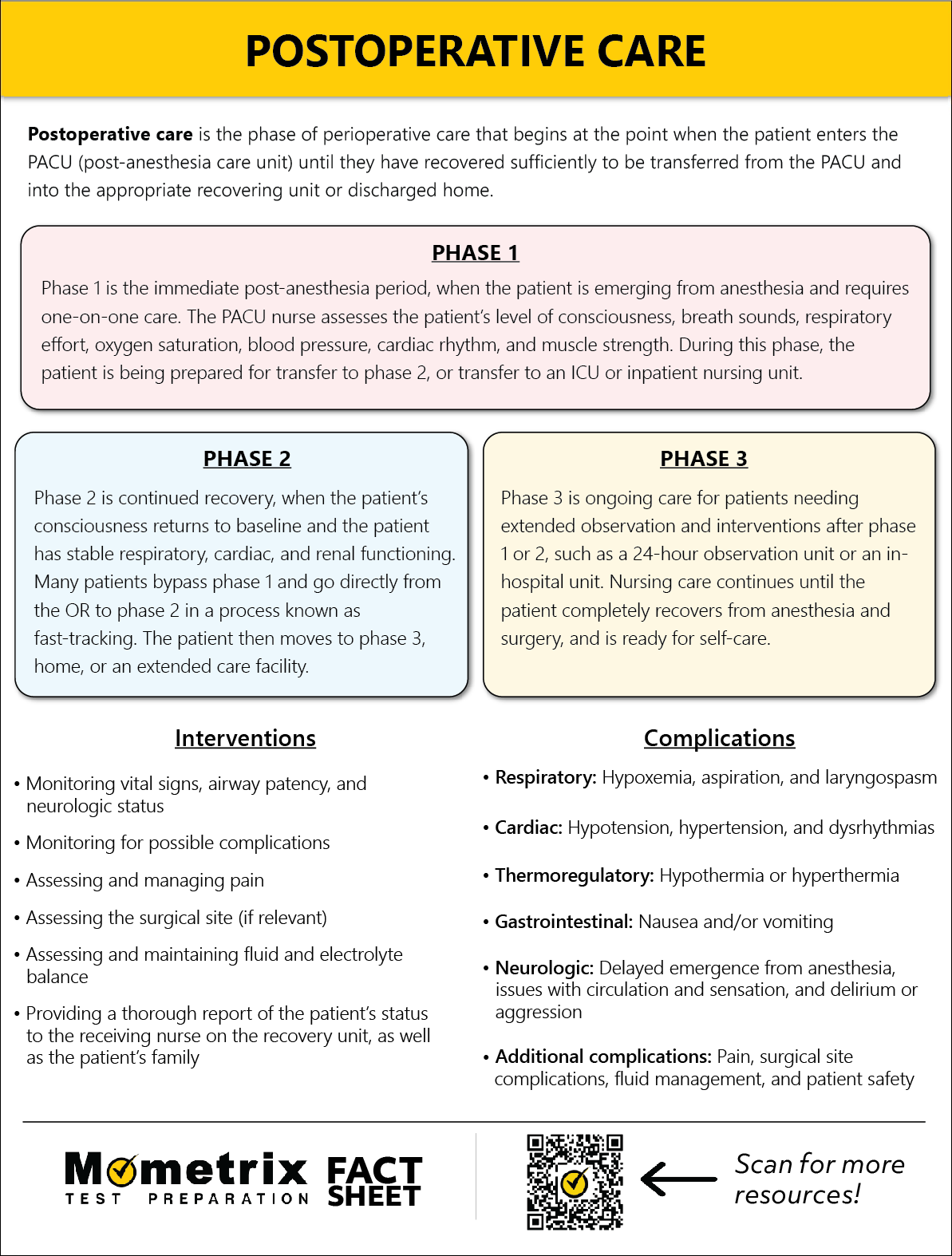
Postoperative Care

Welcome to this video tutorial on postoperative nursing. You may have heard the term “perioperative nursing”—this encompasses the preoperative, intraoperative, and postoperative phases of the patient’s surgical experience. This video will focus on the postoperative phase, which begins with the patient’s admission to the postanesthesia care unit (PACU) and ends once the anesthesia has worn off enough for the patient to be safely transferred to the appropriate nursing unit.
Nursing Interventions
The postanesthesia nurse must understand the patient’s risks for complications and be prepared to implement interventions should there be a change in the patient’s status.
Nursing interventions include monitoring vital signs, airway patency, and neurologic status; managing pain; assessing the surgical site; assessing and maintaining fluid and electrolyte balance; and providing a thorough report of the patient’s status to the receiving nurse on the unit, as well as the patient’s family.
Post-Anesthesia Care Unit (PACU)
The patient must be stable and free from symptoms of complications in order to transfer from the PACU to the clinical unit or home. However, the potential for developing complications goes beyond the immediate postoperative phase and ongoing nursing assessment is essential on the postoperative nursing floor as well. In this video, we will be focusing on the immediate postoperative care in the PACU.
The PACU should be located near the operating rooms. It is usually a large open room, divided into individual patient care spaces. There are usually 1.5 to 2 patient care spaces per operating room. Each patient care space is supplied with a blood pressure monitoring device, cardiac monitor, pulse oximeter, oxygen, airway management equipment, and suction. Emergency equipment and medications are often centrally located.
The length of stay in the PACU is determined on a case-by-case basis, there is not a mandated minimum stay requirement. The American Society of PeriAnesthesia Nurses (ASPAN) recommends that critically ill patients do not recover in the same area as ambulatory surgical patients.
Registered nurses in the PACU demonstrate in-depth knowledge of patient responses to anesthetic agents, surgical procedures, pain management, and potential complications.
Stages of Post-Anesthesia Care
There are three phases of postanesthesia care.
Phase 1 is the immediate post-anesthesia period, when the patient is emerging from anesthesia and requires one-on-one care. The PACU nurse assesses the level of consciousness, breath sounds, respiratory effort, oxygen saturation, blood pressure, cardiac rhythm, and muscle strength. The patient is being prepared for transfer to phase 2, ICU, or an inpatient nursing unit.
Phase 2 is continued recovery; when the patient’s consciousness returns to baseline and the patient has stable pulmonary, cardiac, and renal functioning. Many patients bypass phase 1 and go directly from the OR to phase 2; this process is known as “fast-tracking.” The patient then moves to phase 3, home, or an extended care facility.
Phase 3 is ongoing care for patients needing extended observation and intervention after phase 1 or 2, such as a 23-hour observation unit or in-hospital unit. Nursing care continues until the patient completely recovers from anesthesia and surgery and is ready for self-care.
Patient Assessment
The PACU nurse will receive a detailed verbal report from the circulating OR nurse and/or anesthesiologist that is bringing the patient to recovery. The PACU nurse performs an immediate assessment of the patient’s airway, respiratory, and circulatory status, then focuses on a more thorough assessment. Immediate post-anesthesia nursing care (phase 1) focuses on maintaining ventilation and circulation, monitoring oxygenation and level of consciousness, preventing shock, and managing pain. The nurse should assess and document respiratory, circulatory, and neurologic functions frequently.
Neurologic functions can be assessed by the patient’s response to verbal stimuli, pupils’ responsiveness to light and accommodation, ability to move all extremities, and strength and equality of a hand grip. A level of consciousness assessment is also helpful, such as the AVPU scale or the Glasgow Coma Scale. The AVPU scale assesses if the patient is alert and oriented, responds to voice, responds to pain, or is unresponsive. The Glasgow Coma Scale is an objective way to record the conscious state of a patient, examining eye, verbal, and motor responses. The lowest possible score is 3, indicating deep coma or death, while the highest score is 15, a fully awake person.
Assessment of the respiratory status may include pulse oximetry, arterial blood gases, and chest x-ray. Respiratory complications exist for all patients and include airway obstruction, hypoxemia, hypoventilation, aspiration, and laryngospasm. Airway obstruction is a serious complication after general anesthesia, and commonly results from the movement of the tongue into the posterior pharynx; changes in the pharyngeal and laryngeal muscle tone; or laryngospasm, edema, and secretions of fluid collecting in the pharynx, bronchial tree, or trachea. Symptoms include gurgling, wheezing, stridor, retractions, hypoxemia, and hypercapnia.
Treatment includes administering 100% oxygen, suctioning of secretions, jaw-thrust maneuver to maintain airway, and insertion of an oral or nasal airway. If none of these interventions are successful, then endotracheal intubation, cricothyroidotomy, or tracheostomy may be necessary. Patients with obstructive sleep apnea have a complete or partial collapse of the pharynx during inspiration and are at an increased risk of airway obstruction from the effects of anesthesia. They are also at risk for hypoxemia because of the residual effects of anesthetic agents. The nurse should monitor the patient for apnea and dysrhythmias and continuously monitor oxygen saturation.
Hypoxemia is a common complication in the immediate postoperative period when pulse oximetry is less than 90% and PO2 is less than 60 mmHg per ABG. It may be a result of hypoventilation, related to:
- Opioids – causing respiratory center depression
- General anesthesia
- Insufficient reversal of neuromuscular blocking agents – resulting in residual muscle paralysis
- Increased tissue resistance – from emphysema or infections
- Decreased lung and chest wall compliance – from pneumonia
- Obesity or gastric and abdominal distention
- Incision site close to the diaphragm
- Constrictive dressings
- Postoperative pain
Aspiration is when gastric contents or blood is inhaled into the tracheobronchial system. It is usually caused by regurgitation; however, blood may result from trauma or surgical manipulation. Risk for aspiration is the reason patients need to be NPO prior to surgery, so there is nothing in the stomach. Aspiration of gastric contents can cause pneumonitis, chemical irritation, destruction of tracheobronchial mucosa, and secondary infection.
Laryngospasm is another respiratory complication, in which the laryngeal muscle tissue spasms, and causes a complete or partial closure of the vocal cords, resulting in airway obstruction. If not treated, laryngospasm can result in hypoxia, cerebral damage, and death. If the patient is extubated too quickly, they are at risk for airway spasm, aspiration, coughing, and airway obstruction. If there is repeated suctioning and irritation by the ET tube or artificial airway, laryngospasm can occur after extubation. Symptoms of laryngospasm include dyspnea, crowing sounds, hypoxemia, and hypercapnia. Treatment includes removing the irritating stimulus, hyperextending the patient’s neck, elevating the head of the bed, giving oxygen, suctioning if necessary, and positive pressure ventilation by bag and mask. Medication may be given to reduce swelling and airway irritation, or a muscle relaxant may be needed. Re-intubating is only done as a last resort.
Maintaining circulation and assessing for cardiac complications in the immediate post-op period is a priority for nursing care. The most commonly encountered cardiovascular complications are hypotension, hypertension, and cardiac dysrhythmias that occur as a result of anesthetic agents affecting the central nervous system, myocardium, and peripheral vascular system. The signs of hypotension include increased heart rate, systolic pressure of 90 mmHg or less, decreased urinary output, pale extremities, confusion, and restlessness. A common cause of postoperative hypotension is blood loss or inadequate fluid replacement. The PACU nurse should be ready to return the patient to the OR if excessive bleeding or hemorrhage occurs.
Hypertension can also occur postoperatively, due to pain, pre-existing hypertension, sympathetic stimulation, bladder distention, anxiety, or reflex vasoconstriction due to hypoxia, hypercarbia, or hyperthermia. Untreated hypertension may lead to cardiac dysrhythmias, left ventricular failure, myocardial ischemia and infarction, pulmonary edema, and cerebrovascular accident. The hypertension must be adequately treated before the patient is discharged from the PACU.
Cardiac dysrhythmias commonly occurring in the immediate postoperative period include sinus tachycardia, sinus bradycardia, and supraventricular and ventricular dysrhythmias. The nurse should assess for airway patency, adequate ventilation, and administer medications and supplemental oxygen as needed. A crash cart should be readily available.
The PACU nurse is also responsible for monitoring the patient’s temperature, as normal thermoregulation is often disrupted due to medication, anesthesia, and the stress of surgery. Many patients experience hypothermia, which can extend recovery, delay wound healing, and increase postoperative morbidity. Shivering increases oxygen demands up to 400%, which results in an increased metabolic rate and myocardial workload. Hypothermia also impairs coagulation, causes decreased cerebral blood flow, and vasoconstriction. Signs of hypothermia include shivering, tachypnea, and tachycardia. Rewarming is essential in the immediate postoperative care of the patient in PACU.
Hyperthermia, when core temp gets above 102.2°F, may be caused by infection, sepsis, or malignant hyperthermia, which can occur for 24-72 hours after surgery. If unrecognized or untreated, malignant hyperthermia results in death.
Fluids are lost during surgery through blood loss, hyperventilation, and exposed skin surfaces. Volume may be replaced with IV fluids, and excessive blood loss replaced with blood, blood products, colloids, or crystalloids. The body naturally retains fluid for at least 24 to 48 hours after surgery, due to the stimulation of antidiuretic hormone as part of the stress response and the effects of anesthesia. The patient should be monitored for fluid and electrolyte imbalances, pulmonary edema, and water intoxication. Fluid intake usually exceeds output during the first 24 to 48 hours. Even if the IV fluid intake is 2,000-3,000 mL, the first void may not be more than 200 mL, and total urinary output for the surgery day may be less than 1500 mL. As the body stabilizes, fluid and electrolyte balance returns to normal within 48 hours.
Nausea and vomiting is a common postoperative problem and can also lead to fluid and electrolyte imbalance. It is often caused by the effects of general anesthesia, abdominal surgery, opiate analgesics, and history of motion sickness. Nausea and vomiting usually occurs in the first 24 hours, with the highest incidence in the first 2 hours. It can prolong recovery time, sometimes resulting in an unplanned hospital admission for an outpatient surgery patient.
Pain is a common occurrence after most all types of surgical procedures and is probably the most significant postoperative problem in the eyes of the patient. Prompt and adequate pain relief is a critical nursing intervention. Unresolved acute pain has many negative effects, including more complications, longer hospital stays, greater disabilities, and the potential for chronic pain. There is an association between high pain scores and nausea, respiratory complications, slower return of GI function, and increased risk of DVT. Effective methods of postoperative pain relief include preemptive analgesia (which is given prior to surgery or prior to pain), giving around-the-clock analgesics, PCA (patient-controlled analgesia, PRN (as needed) dosing, management of breakthrough pain, and nonpharmacologic interventions. Assessment of the patient’s pain is the first priority. The patient’s report is the most reliable indicator of pain intensity, and using a numeric or faces pain rating scale is a reliable tool.
Other important assessments include:
- Surgical site – dressing dry and intact
- Proper draining of drainage tubes
- Rate and patency of IV fluids
- Level of sensation after regional anesthesia
- Circulation/sensation in extremities after orthopedic or vascular surgery
- Patient safety
During the patient’s stay in PACU, the nurse documents all assessments and interventions. Patients usually remain in the PACU until their vital signs are stable and they are reasonably capable of self-care. Discharge from the PACU is usually determined by a numeric scoring system; the most common one in use is the Aldrete score. There is a phase 1 Aldrete score that measures activity, respiration, circulation, consciousness, and oxygen saturation (or color). Each measurement is scored from 0 to 2, with a total score of 9 or 10 qualifying for discharge from the PACU.
Patient Discharge
The anesthesiologist often discharges the patient from phase I. The phase II Aldrete score is used for patients who are conscious or those who received local or regional anesthesia, and have moved on from phase I. The patient will then be discharged home, a short-stay unit, or an inpatient unit. If the patient is staying in the hospital unit, the PACU nurse gives a report to the nurse on the inpatient unit who will take over care of the patient.
When the patient moves to the inpatient unit or short-stay unit, they are in the 3rd phase of postanesthesia care: ongoing postoperative care.
Review
Here’s a question to get you thinking…
The nurse in the PACU suspects laryngospasm in the patient who develops which of the following symptoms?
- Decreased oral secretions
- Sternal retractions
- Crowing sounds
- Hypocapnia
Thank you for watching this video tutorial on postoperative nursing!
Frequently Asked Questions
Q
What is postoperative/post-anesthesia care?
A
Postoperative care is the care that is provided outside the operating room in the post-anesthesia care unit during the period in which the patient is recovering from anesthesia. The patient remains in the postanesthesia care unit (PACU) until stable, but postoperative monitoring continues on the nursing unit after transfer until eventual discharge.
Q
What are the three phases of postoperative/post-anesthesia care?
A
The three phases of postoperative/postanesthesia care are as follows:
- Phase 1: Immediate post-anesthesia care in the PACU with monitoring of the patient’s level of consciousness, physical status, and vital signs. Some patients may bypass phase 1 and go immediately to phase 2 (fast-tracking).
- Phase 2: Continued recovery with consciousness and physical functioning returning to baseline and the patient demonstrating readiness for transfer to home or an extended care facility.
- Phase 3: Ongoing observation (if necessary) after phase 1 and 2 until the patient is fully recovered. This may be performed in a 24-hour unit or a hospital inpatient unit, and lasts until the patient is capable of their baseline level of self-care.
Q
What nursing interventions are required in postoperative care?
A
Nursing interventions that are required in postoperative care include prompt pain control, assessment of the surgical site and drainage tubes, monitoring the rate and patency of IV fluids and IV access, and assessing the patient’s level of sensation, circulation, and safety. Other interventions include monitoring vital signs, airway patency, and neurologic status in addition to maintaining fluid and electrolyte balance.
Q
What are common respiratory complications that can occur in the postoperative phase of care?
A
Common postoperative respiratory complications include:
- Airway obstruction, commonly due to excessive secretions.
- Hypoventilation, resulting from delayed emergence from anesthesia.
- Hypoxemia, indicated if the patient’s oxygen saturation is <90% and PO2 is <60mmHg.
- Aspiration on secretions or vomit.
- Laryngospasm, the spasming of the vocal cords secondary to endotracheal extubation.
Q
What are common cardiac complications that can occur in the postoperative phase of care?
A
Common postoperative cardiac complications include:
- Hypotension: A systolic blood pressure of <90 mmHg, which may be secondary to anesthesia, or may indicate excessive blood loss, active bleeding, or other complications that must be further investigated.
- Hypertension: A systolic blood pressure of >160 mmHg, which is usually transient in nature.
- Cardiac dysrhythmias: May include sinus tachycardia, sinus bradycardia, and supraventricular and ventricular dysrhythmias.
Q
What are common thermoregulatory complications that can occur in the postoperative phase of care?
A
Common thermoregulatory complications that can occur in the postoperative phase of care include the following:
- Hypothermia (a core temperature less than 36 °C) can cause impaired coagulation, decreased cerebral blood flow, and vasoconstriction and may result from large volumes of cool IV fluids administered pre- and intra-operatively, reactions to anesthesia, and/or exposure to cool temperatures in the procedure room in conjunction with exposed skin.
- Hyperthermia (a core temperature above 39 °C) may indicate a severe and dangerous complication known as malignant hyperthermia. Malignant hyperthermia results from a dangerous reaction to the anesthetic agents and, if untreated, can lead to death.
Q
What are common gastrointestinal complications that can occur in the postoperative phase of care?
A
Nausea and vomiting are common gastrointestinal complications in the postoperative phase of care and may be a reaction to anesthesia or indicate other complications. Nausea and vomiting are most common in the first 2 hours postoperatively, but may persist for 24 hours. The postoperative nurse must assess for and treat nausea/vomiting to prevent complications associated with vomiting, such as aspiration. Emesis basins/bags should be readily available, anti-nausea medications should be administered intravenously, and the patient sat up or turned on their side if vomiting is imminent.
Q
What are common neurologic complications that can occur in the postoperative phase of care?
A
Common neurologic complications in the postoperative phase of care include delayed emergence from anesthesia (generally defined as requiring greater than 30 to 60 minutes to awaken after anesthesia), impaired level of consciousness, and delirium. Delirium may produce agitation and aggressive behavior. In the case of delirium-induced aggression, the nurse must take precautions for their own safety, and the safety of the patient.
Q
What are common complications related to pain, surgical sites, and patient safety that can occur in the postoperative phase of care?
A
Additional common postoperative complications can be related to the following:
- Pain: Delayed recovery with prolonged pain symptoms, leading to anxiety and distress.
- Surgical sites: Monitor for blocked drainage tubes, bleeding, infection, or dehiscence (rare).
- Patient safety: Falls, hypervolemia, or hypovolemia.
Q
What is required for a patient to be discharged out of postoperative care?
A
The Aldrete score is a standardized tool used to measure a patient’s readiness for discharge from the PACU. The score assesses the patient’s activity, respirations, circulation, consciousness, and oxygen saturation on a scale of 0-2 for each parameter. For discharge from postoperative care, the patient’s Aldrete score should be 9 to 10.
Fact Sheet