Pneumothorax

Hi, and welcome to this review of pneumothorax! Today, we’ll be looking at the causes, signs and symptoms of this condition, as well as what treatment options are available. Let’s get started!
First thing’s first: What is a pneumothorax? A pneumothorax is very simply a collapsed lung. It occurs when air is able to enter the space between the lung and the chest wall, causing the lung to deflate. The change in pressure caused by an opening in your chest or lung wall can cause the lung to collapse and put pressure on the heart.
There are several different possible causes of ruptured or injured chest or lung walls, including lung disease, injury from a sport or accident, assisted breathing with a ventilator, or even changes in air pressure that you experience when scuba diving or mountain climbing. Sometimes the cause of a pneumothorax is unknown.
There are two broad types of pneumothorax: traumatic and non-traumatic. Either type can lead to a tension pneumothorax if the air surrounding the lung increases in pressure. A tension pneumothorax is common in cases of trauma and requires emergency medical treatment. Let’s compare traumatic and non-traumatic.
Traumatic Pneumothorax
A traumatic pneumothorax can be caused by trauma (hence the name) or injury causing air and fluid to leak into the pleural space, collapsing the lung. Trauma may include: motor vehicle accidents, contact sports, which could result in chest trauma, stab wounds or gunshot wounds to the chest, and some medical procedures such as central line placement, ventilator use, lung biopsies, and even CPR.
It’s critical that a pneumothorax caused by significant chest trauma is treated quickly. The symptoms are often severe, and they could contribute to potentially fatal complications such as cardiac arrest, respiratory failure, shock, and death.
Non-traumatic Pneumothorax
A non-traumatic pneumothorax happens without an injury; in fact, it often occurs “spontaneously” and has been given the name spontaneous pneumothorax. Non-traumatic or spontaneous pneumothorax is further broken down into two types: primary and secondary.
Primary occurs in people with no known lung disease. This type is more common in young men who are tall and thin. Secondary pneumothorax typically occurs in older people with known lung disease. This could include:
- Chronic obstructive pulmonary disease (COPD), such as emphysema or chronic bronchitis
- Acute or chronic infection, such as tuberculosis or pneumonia
- Lung cancer
- Cystic fibrosis, a genetic lung disease that causes mucus to build up in the lungs
- Asthma, a chronic obstructive airway disease that causes inflammation
Spontaneous hemopneumothorax (SHP) is a rare subtype of spontaneous pneumothorax. It occurs when both blood and air fill the pleural cavity without any recent trauma or history of lung disease.
The overall signs and symptoms of pneumothorax are usually a sudden chest pain and shortness of breath, also known as dyspnea, but the patient can also have a steady ache in the chest, break out in a cold sweat, experience tightness in the chest, cyanosis (turning blue), and severe tachycardia.
Diagnosis may be picked up by listening to the lungs with a stethoscope, but it can be difficult to determine a pneumothorax if it is particularly small. Generally, a pneumothorax is diagnosed using a chest X-ray. A CT scan may be used in some cases to provide more detailed images, or a thoracic ultrasound may also be used.
Once a pneumothorax is diagnosed, there are several different options available for treatment, depending on the type and severity of the case. Observation or “watchful waiting” is typically recommended for those with a small primary spontaneous pneumothorax (PSP) and who aren’t short of breath. In this case, you should monitor the patient’s condition on a regular basis as the air absorbs from the pleural space. Frequent x-rays need to be taken to check if the affected lung has fully expanded again. It’s best to instruct the patient to avoid air travel until the pneumothorax has completely resolved.
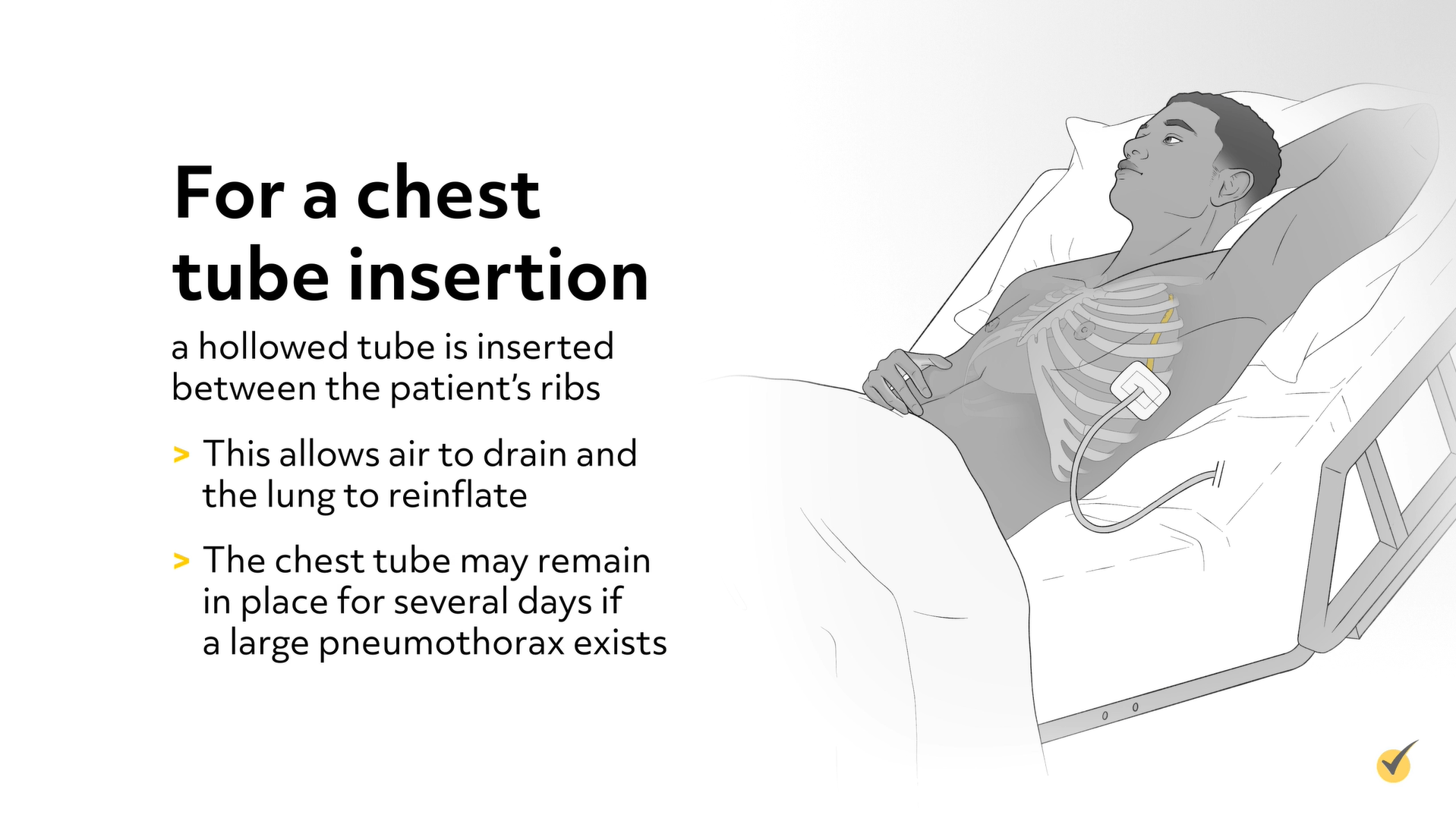
Needle aspiration and chest tube insertion are two procedures designed to remove excess air from the pleural space in the chest. These can be done at the bedside without requiring general anesthesia. Needle aspiration may be more comfortable than placement of a chest tube, but it’s also more likely to require multiple insertions.
For a chest tube insertion, a hollowed tube is inserted between the patient’s ribs. This allows air to drain and the lung to reinflate. The chest tube may remain in place for several days if a large pneumothorax exists.
Pleurodesis may be recommended for a patient who has had repeated pneumothorax as a way of preventing recurrence. The procedure involves using a mildly irritant chemical to obliterate the pleural cavity, which will prevent fluid buildup and prevent a future pneumothorax.
A thoracotomy may be required in certain severe cases of pneumothorax when a large amount of air is trapped or in certain lung conditions. A thoracotomy involves cutting into the pleural space to see what’s going on and make repairs as necessary. The lung, in part or whole, may be removed during this procedure.
Thoracoscopy, also known as video-assisted thoracoscopic surgery, or VATS, is performed by inserting a tiny camera through the chest wall to view the affected area. A thoracoscopy can help you decide what treatment is best for that particular case. The possibilities include sewing blisters closed, closing air leaks, or removing the collapsed portion of the lung. Depending on the severity of the case and the selected route of treatment, a patient affected by a pneumothorax might take anywhere from 2 weeks to 2-3 months to fully recover.
Okay, before we go, let’s go over a couple of review questions to test your memory.
Review Questions
1. Which of the following are possible symptoms of a pneumothorax?
- Bloating and weight gain
- Longer expiration
- Coughing up blood
- Tachycardia
Typical, general symptoms may include sudden chest pain and dyspnea, but the patient can also have a steady ache in the chest, break out in a cold sweat, experience tightness in the chest, cyanosis, and severe tachycardia.
2. Which of the following is a preferred treatment option for a more severe case of pneumothorax?
- Pleurodesis
- Thoracotomy
- Needle aspiration
- Chest tube insertion
Pleurodesis may be recommended for a patient who has repeated pneumothorax, while needle aspiration and chest tube insertion are procedures designed to remove excess air from the pleural space in the chest.
That’s all for this review! Thanks for watching, and happy studying!
