
Welcome to this video about fall prevention!
It’s estimated that 25% of people 65 and older fall every year with over 3 million requiring treatment in an emergency department and 950,000 requiring hospitalizations. Falls are the most common cause of hip fractures and traumatic brain injuries in this demographic.
Not only are the human costs of falls high, but the cost of care in dollars is more than $50 billion a year. Therefore, screening for fall risk and utilizing fall prevention measures are essential.
STEADI
The Centers for Disease Control and Prevention has developed the STEADI algorithm for fall risk. STEADI stands for Stopping Elderly Accidents, Deaths, and Injuries. There are three steps to the algorithm: screening, assessment, and interventions.
The first step in the STEADI algorithm is to screen. Screening for risk factors should be done yearly or any time a patient experiences an acute fall. The screening tool that the CDC recommends is called “Stay Independent” and consists of 12 statements, to which the person answers “yes” or “no.”
If the person responds “yes” to four or more of these statements, this indicates that the person is at risk of falls. If the person responds “yes” to fewer than four but has actually experienced a fall within the past year, the person is also at risk.
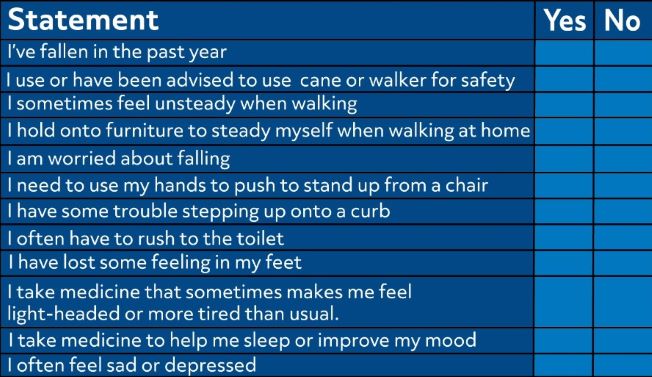
The three key issues that indicate the most risk for falls are:
- Feeling unsteady when standing or walking
- Worrying about falling
- Falling in the past year
If any of these three key issues are present, it’s important to ask how often they have occurred and if the person experienced any injury.
If the screening indicates that the person is not at risk, this is an excellent time to educate the individual about fall prevention and to assess vitamin D intake to ensure that it’s adequate for bone health.
Assessing Modifiable Risk Factors and Fall History
If the screening indicates that the individual is at risk, then the next step in the STEADI algorithm is to assess the person’s modifiable risk factors and history of falls. There are eight elements to assess, and these assessments should be followed by the appropriate interventions.
Assessment #1
First, evaluate gait, strength, and balance. Assessment tools may include:
- The timed up-and-go test
- The 30-second chair stand
- The four-stage balance test
If there is evidence of poor gait, decreased strength, or poor balance, then the interventions may include a referral for physical therapy and/or evidence-based exercise or fall prevention programs. Some individuals may require assistive devices, such as walkers or canes.
Assessment #2
Identify medications that increase fall risk in older adults by referring to the American Geriatrics Society Beers Criteria for Potentially Inappropriate Medications Use in Older Adults, usually just referred to as the Beers Criteria.
Some of the medications that increase risk include:
- First generation antihistamines, such as diphenhydramine (better known as Benadryl)
- Cardiovascular drugs, such as doxazosin and terazosin, clonidine, nifedipine, and amiodarone
- Antidepressants, such as amitriptyline
- Antipsychotics
- Barbiturates
- Benzodiazepines
- Long-acting sulfonylureas
- Metoclopramide
- NSAIDs (secondary to the bleeding risks involved)
- Proton pump inhibitors
- Muscle relaxants
If the individual is taking a medication that increases risks of falls, the healthcare provider should consider discontinuing, switching, or decreasing the dosage. If this isn’t possible, then the individual should be made aware of the possible issues with the medications and given precautions to avoid falls.
Assessment #3
Ask about potential hazards in the home, such as poor lighting, throw rugs, slippery floors, slippery tubs, and lack of handrails on stairs. If there are environmental hazards, then the appropriate intervention is to refer to an occupational therapist who can evaluate the home for safety issues and make recommendations, such as:
- Installing non-slip flooring
- Installing grab bars and handrails
- Improving lighting
- Removing clutter
- Securing carpets, removing throw rugs, and repairing flooring.
Assessment #4
Assess the individual’s blood pressure in both the standing and lying positions to determine the presence of orthostatic hypotension. Blood pressure normally changes with position change, but if the drop is excessive, the individual can become light-headed or even faint.
If the individual’s systolic blood pressure drops more than 20 millimeters of mercury or their diastolic blood pressure drops more than 10 millimeters of mercury upon standing, this is an indication of orthostatic hypotension.
If the individual exhibits orthostatic hypotension, then interventions may include stopping, switching, or reducing medications that are causing it; encouraging exercise; applying compression stockings; encouraging adequate hydration; and establishing blood pressure goals.
Assessment #5
Check visual acuity with the Snellen eye test, which can detect changes in visual acuity, such as may occur with cataracts. Vision may also be checked with the Amsler chart, which is a grid that can help to detect visual distortions, a first sign of macular degeneration.
If there is evidence of visual changes, then the intervention is to refer the person to an ophthalmologist for examination. If a medication may be causing the visual disturbances, then it may need to be stopped, switched, or reduced if possible.
Assessment #6
Assess the individual’s feet and footwear to determine if the feet are healthy or have abnormalities, such as bunions, ulcerations, or hammertoes and if the shoes are fitted properly and are safe to walk in.
If foot abnormalities are present, then the individual should be referred to a podiatrist. If shoe problems are noted, such as slick soles or slip-on shoes, the appropriate intervention is to educate the individual about shoe fit, traction, insoles, and heel height and refer them to a podiatrist.
For older adults at risk for falls, interventions with regards to footwear include recommending the following:
- A supported heel collar for stability
- Shoelaces or Velcro fasteners to ensure a snug fit
- A low heel height and an angled heel
- Thin, hard, non-slip soles
Assessment #7
Assess vitamin D intake with a blood test. The normal range for vitamin D, 25 hydroxy is 30 to 70 ng/mL (nanograms per milliliter).
If vitamin D levels are deficient, then the intervention is a daily vitamin D supplement and education about sources of vitamin D (such as exposure to the sun, mushrooms, egg yolks, tuna, fatty fish such as salmon, and spinach), in addition to periodic monitoring. Safe sun exposure is usually considered to be about 20 minutes daily with the arms exposed.
Assessment #8
Identify comorbidities that may contribute to falls, such as depression, confusion, neuromuscular disorders, diabetes, hearing or vision loss, and osteoporosis. The most appropriate intervention is to ensure that the individual is receiving optimal treatment to control the disorder.
The important thing to remember about fall prevention is that most falls can be avoided. It is a failed assumption to believe that falling is an inevitable part of aging. As individuals age, they need to stay active, remove hazards in the home environment, wear appropriate footwear, review their medications, and have regular physical examinations, including hearing and vision examinations, in order to reduce their risk of falls and the resulting complications.
That’s all for now! Thanks for watching, and happy studying!

