Hi, and welcome to this video tutorial about chest tubes. We’re going to look at what a chest tube is and the nursing interventions involved during and after insertion.
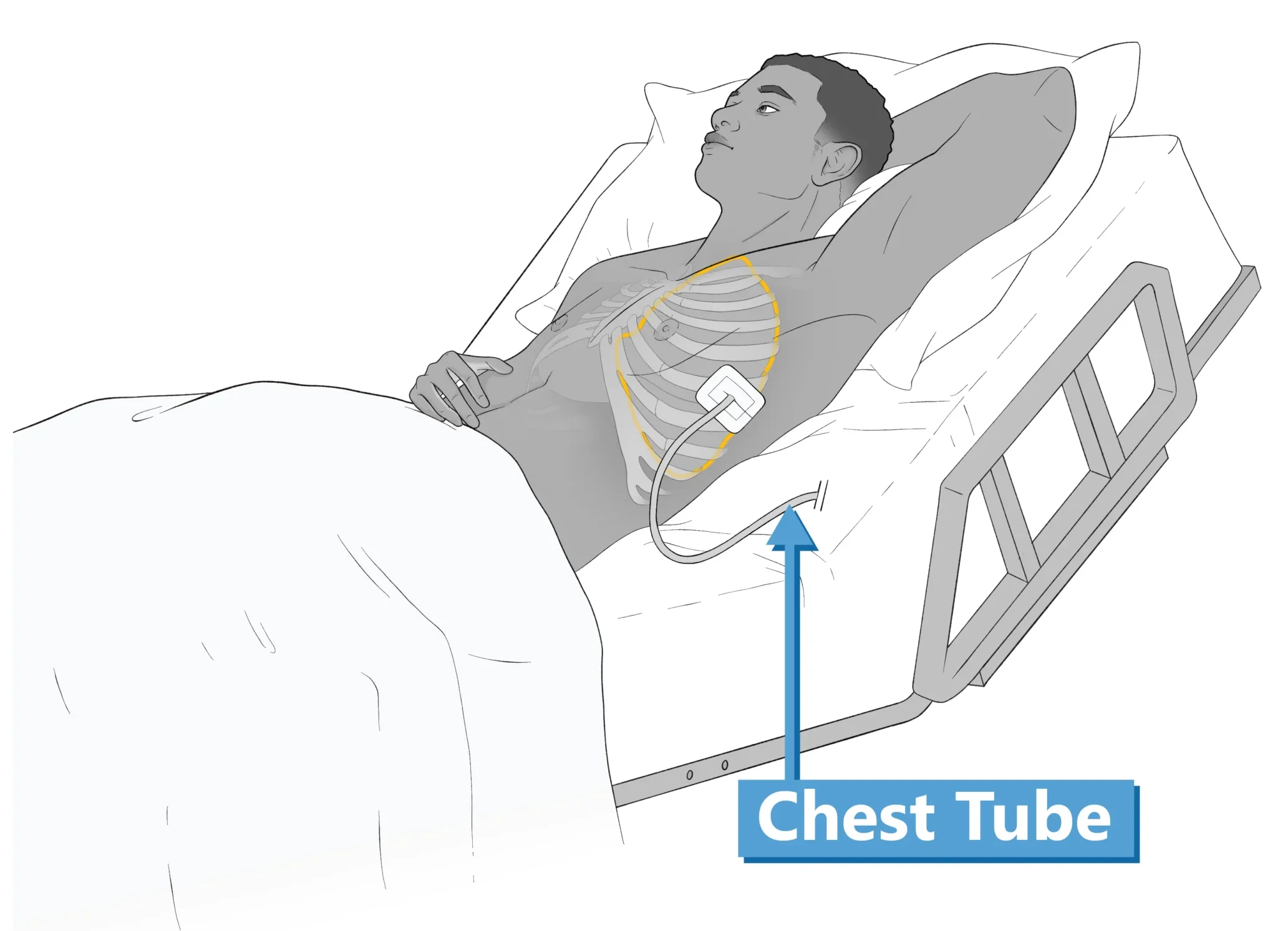
A chest tube is a thin tube inserted through the chest wall, into the space between the visceral pleura and parietal pleura, known as the pleural cavity. They are also known as pleural catheters.
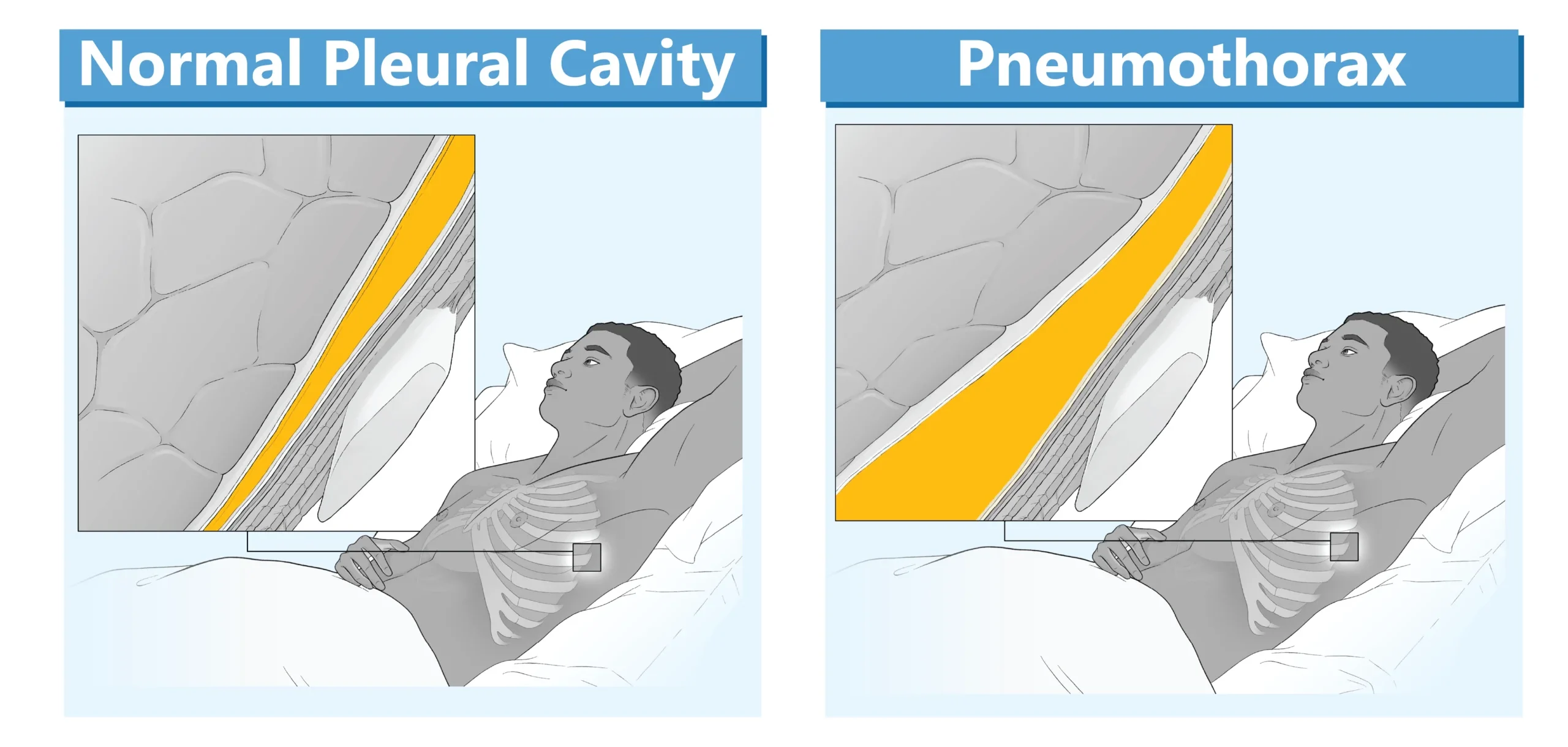
The pleural cavity normally contains a small amount of straw-colored fluid, however, in underlying lung diseases, air or fluid may accumulate in this space. Abnormal accumulation of air in the pleural space is called a pneumothorax and the buildup of blood (hemothorax), pus (empyema), lymph (chylothorax), or serous fluid (pleural) are known as effusions.
Chest Tube Uses
Pressure within the pleural cavity is normally negative, but when air or excess fluid accumulates, it disrupts the normal pressure, preventing the lung from fully expanding. A chest tube is placed to drain the excess fluid or air from the pleural cavity, restoring lung function. Chest tubes are also used to instill chemotherapeutic drugs or sclerosing agents to treat recurrent pleural effusions (a procedure called pleurodesis). Chest tubes may also be used prophylactically after thoracic or cardiac surgery to prevent the accumulation of fluids.
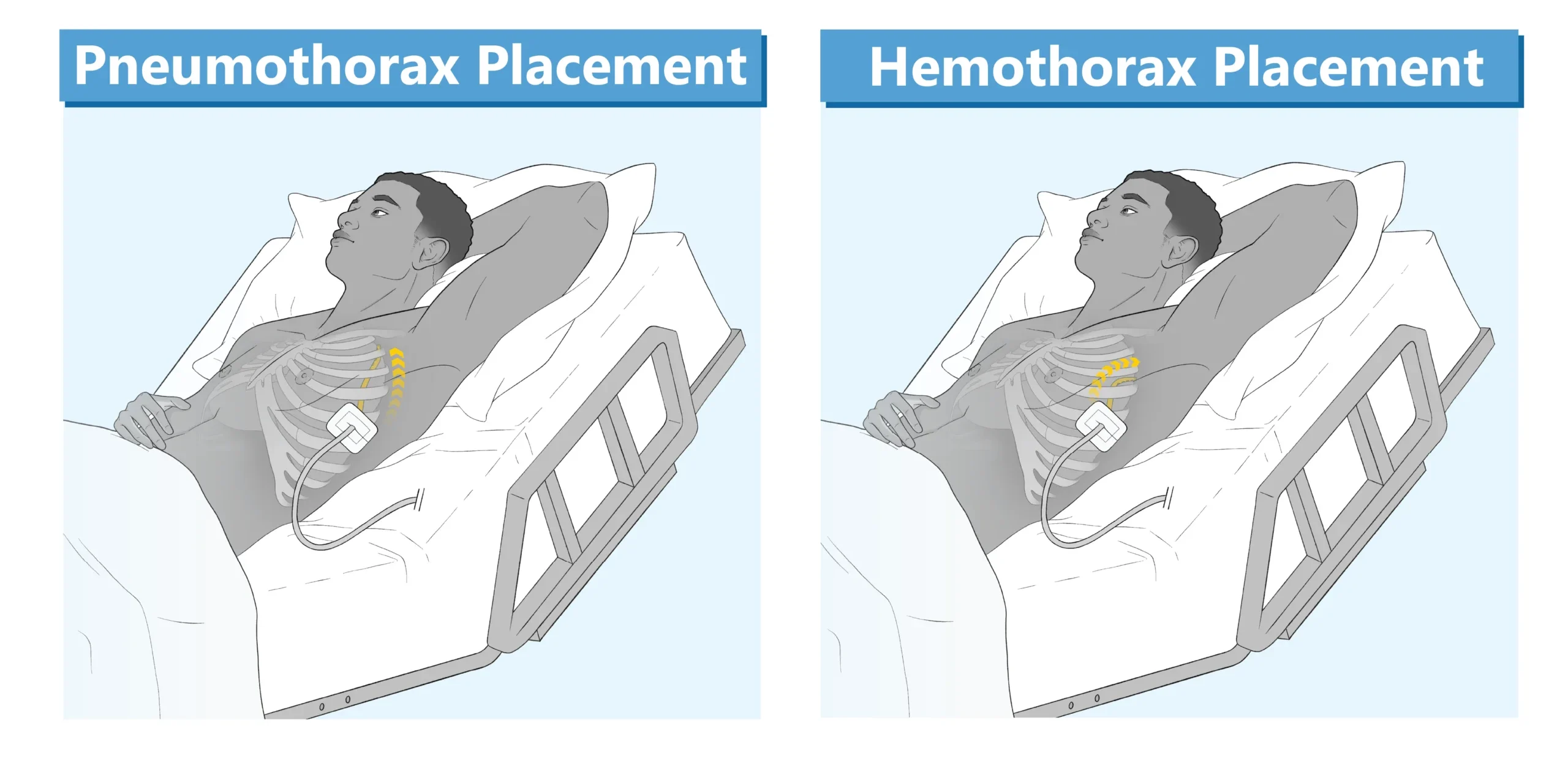
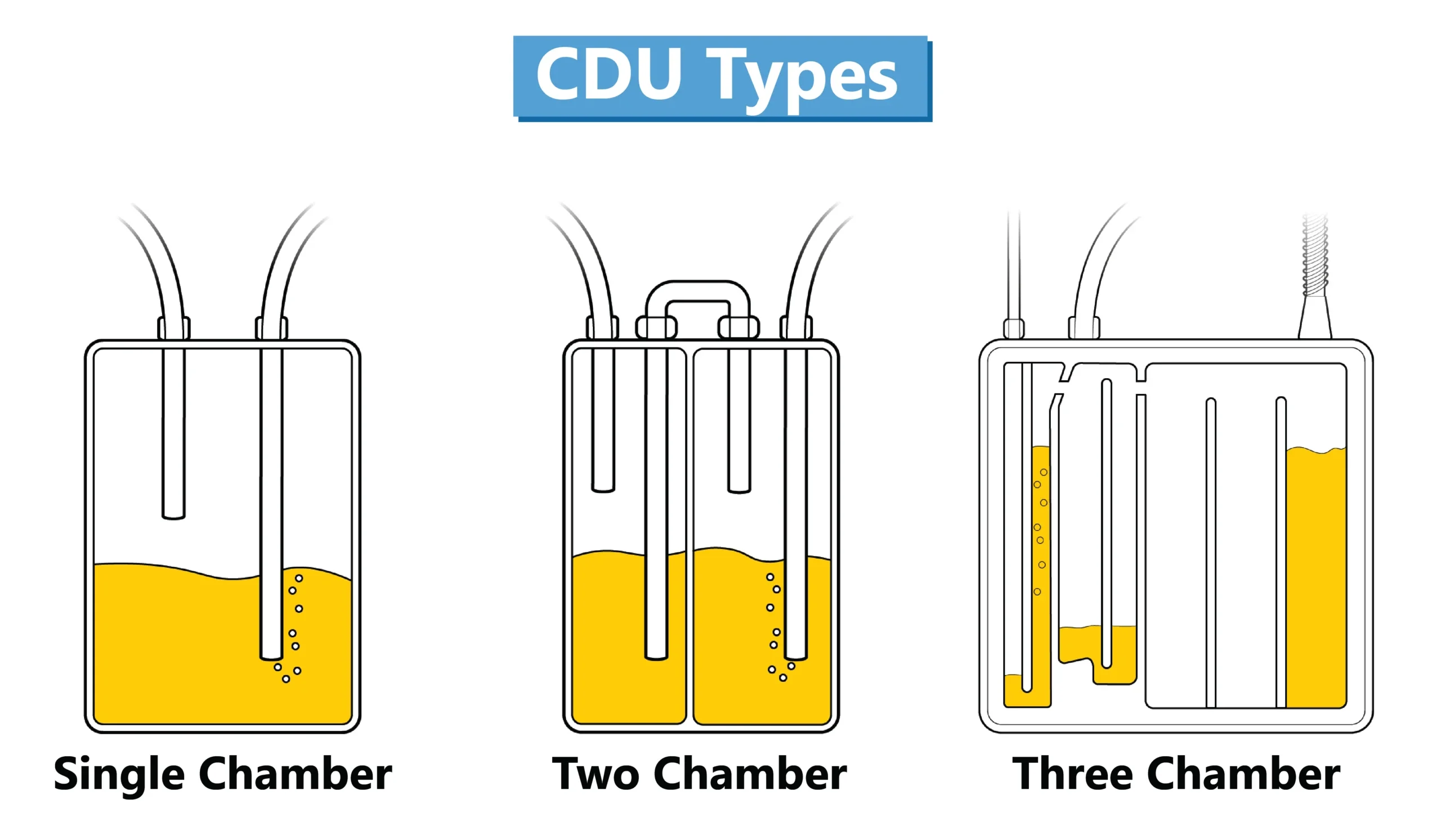
Chest tubes are placed in the pleural space, either percutaneously or surgically. The location is dependent on what is being drained. The tube should be directed high and anterior for a pneumothorax; and for a hemothorax, the tube is usually directed posteriorly and lateral to the nipple line. The chest tube is sutured in place, covered with an occlusive petroleum gauze dressing and attached to a chest drainage unit (CDU). The CDU is used to restore normal intrapleural pressure, facilitate the drainage of air and fluid, and prevent backflow of air. CDUs are categorized according to the number of chambers and mechanisms for preventing air from entering the pleural space.
Chamber Systems
Although single and two-chamber systems are available, systems incorporating three separate chambers, aligned in an integrated unit are widely used.
These systems consist of the following:
- A collection chamber: Fluids from the pleural space drain directly into this chamber via a 6-foot patient tube, which allows monitoring of the characteristics and quantity of drainage.
- A water-seal chamber: Acts as a one-way valve, allowing drainage of air and fluid; prevents air from entering the pleural cavity. The chamber is filled with sterile water (as specified by the manufacturer), which oscillates with inhalation and exhalation (tidaling) reflecting normal pressure.
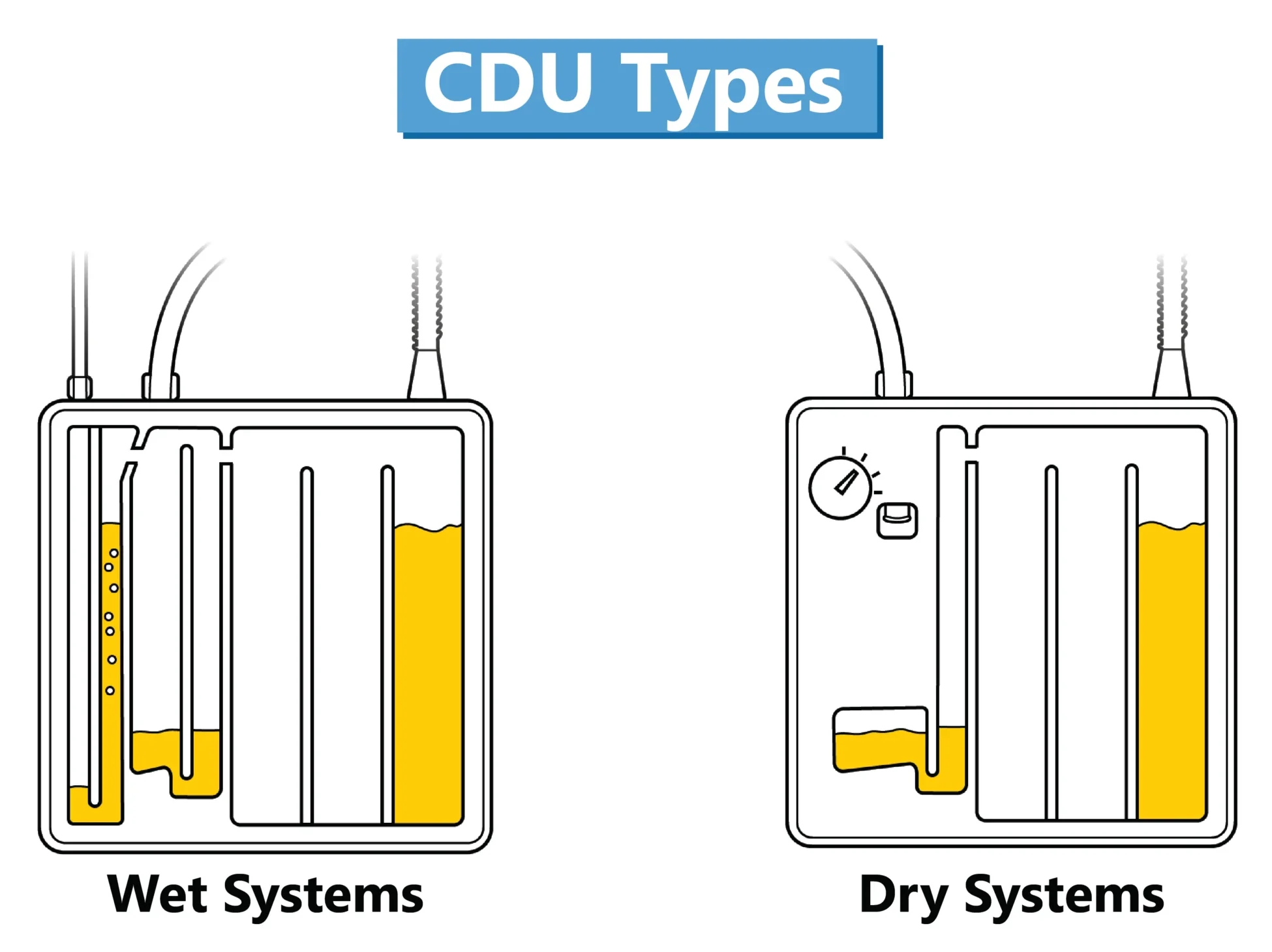
- A suction control chamber regulates the amount of negative pressure generated. Suction control chambers differ in the mechanism utilized to regulate the suction. The suction pressure of “Wet Systems” is regulated by the height of a column of water in the suction control chamber; “Dry Systems” utilize a regulator and a suction monitor bellows, which expands when suction is operating. Suction pressure is commonly set at −20 cm of water.
Nurse Responsibilites and Interventions
When caring for a patient with a chest tube, the nurse is responsible for the following:
- Having core clinical knowledge and skills to perform an appropriate assessment of a patient’s respiratory status; identifying assessment findings outside the normal range; and delivering best practice in chest-tube management.
- Following the facility’s policies/procedures and CDU manufacturer’s recommendations when providing care and documenting clinical assessments, interventions, and patient response.
- Practicing hand hygiene and maintaining aseptic technique when handling equipment.
- and Reporting new or significant changes in the patient’s condition.
There are four main nursing interventions to include:
First is performing ongoing assessments of the patient and equipment according to facility policy for frequency of monitoring vital signs; respiratory status (which includes skin color, respiratory depth, rhythm, use of accessory muscles, 02 saturation, and breath sounds); pain level; insertion site dressing (making sure it’s dry, intact, occlusive, and looking for signs of subcutaneous emphysema); patient drainage and suction tubing (looking for kinks, bends, dependent loops, loose connections air leaks, and patency); wall suction (which is generally set at 80-120 millimeters of Mercury); correct positioning of the CDU; and the presence of emergency equipment in the patient’s room.
Second, you will need to change the insertion site dressing per physician’s orders, assessing the insertion site for signs of infection, displaced chest tube, or subcutaneous emphysema.
Third, you will need to change the CDU when full or not functioning.
Lastly, you will need to educate the patient on frequent position changes, coughing, and deep breathing.
Review Questions
1. Which of the following is not true regarding the purpose of a chest tube?
- Restores negative intrathoracic pressure.
- Removes thick mucus and secretions from the lower airway.
- Removes excess air and fluid from the pleural space.
- Prevents the accumulation of fluid after cardiothoracic surgery.
Chest tubes are placed in the pleural space, not the lower respiratory tract.
2. Which of the following statements about chest tube drainage systems is not true?
- Continuous bubbling in the collection chamber means there is an air leak.
- The oscillation of the water level in the water-seal chamber with the patient’s respirations reflect normal pressure changes in the pleural cavity.
- A suction pressure of -20 cm H2O is commonly recommended for adults.
- In a “wet system”, the amount of suction is controlled by the height of the column of water in the suction control chamber, and not the setting of the suction source.
Continuous bubbling in the water-seal chamber may indicate an air leak.
3. Which assessment finding indicates to a nurse caring for a patient with a chest tube attached to a dry system, that the CDU is functioning effectively:
- Vigorous bubbling in the Water-seal Chamber.
- Redness, purulent drainage or other signs of infection at the chest tube insertion site.
- Fluctuation of water in the patient drainage tubing during inhalation and exhalation.
- The bellows in the suction monitor is expanded.
In a dry system, the bellows located in the suction monitor will expand only when suction is operating.
Thanks for watching, and happy studying!