
Hi, and welcome to this review of cardiac tamponade!
Today, we’ll be going over what this condition is, how it’s diagnosed, what complications arise from it, and how it can be treated.
Let’s get started!
Definitions
First, what is cardiac tamponade? Well, as is often the case with medical names, we can get an idea of what’s going on by analyzing the name of the condition. Cardiac refers to the heart, and tamponade comes from the same French root as our word tampon, which indicates a blockage meant to stop bleeding.
From this, we can assume that we’re dealing with a blockage in or near the heart that cuts off blood flow—and we’d be correct. Cardiac tamponade is a mechanical compression of the heart caused by a buildup of fluid in the pericardial sac, which is the sac that surrounds the heart.
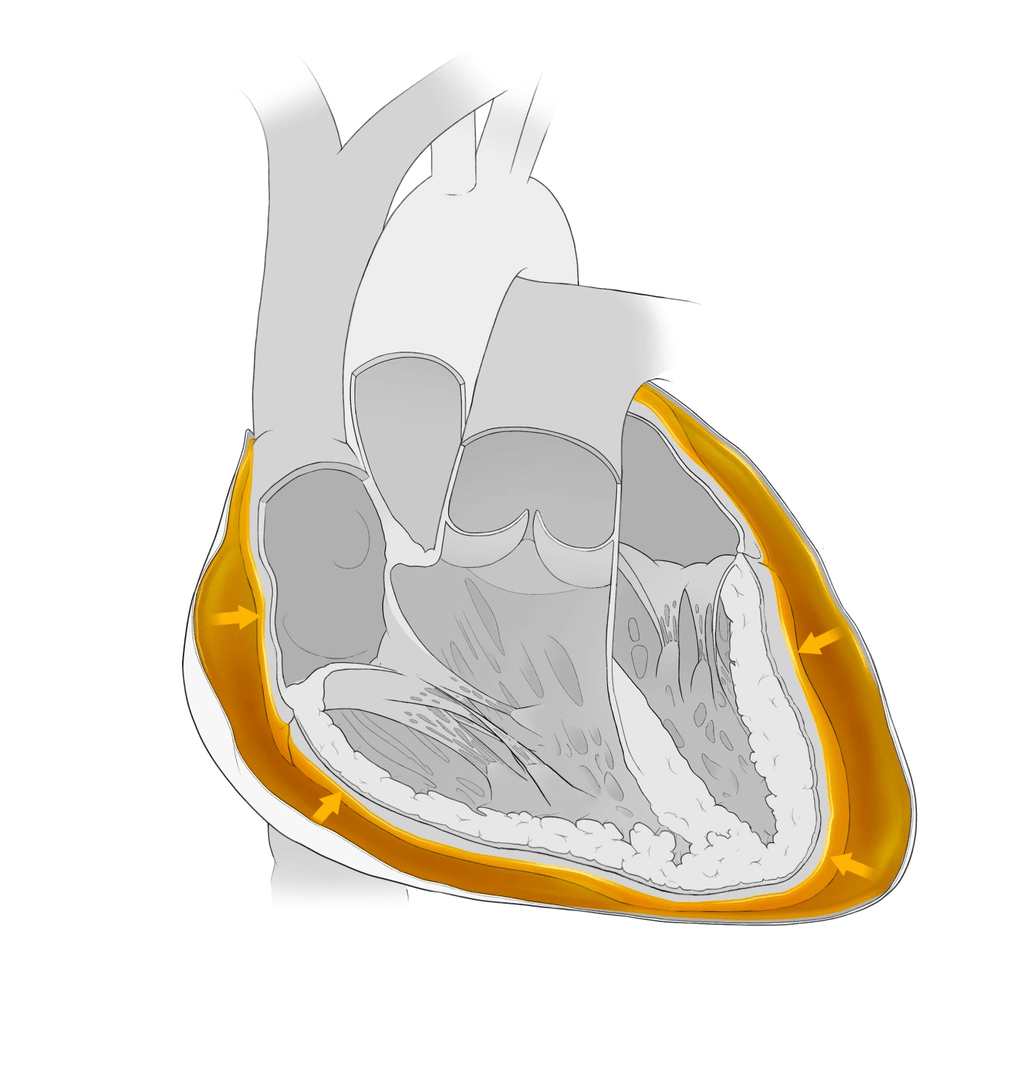
Increased fluid in this sac can exert pressure on the heart muscle, which affects its ability to contract and prevents the chambers from filling with blood. Since this is the pump that supplies blood to the entire body, including the heart muscle itself, this condition can be fatal if left untreated.
But what actually causes this increase in fluid? The most common causes are rupture of an aortic aneurysm, advanced lung cancer, acute pericarditis, a heart attack, and/or heart surgery. A chest injury, such as a stab wound or trauma from a car accident can also cause cardiac tamponade.
Symptoms
As the fluid builds up and movement of the heart is constricted, some of the following symptomatic effects may occur:
- Anxiety and restlessness
- Sharp chest pain radiating to the neck, shoulders, or back
- Trouble breathing or taking deep breaths
- Rapid breathing
- Discomfort that’s relieved by sitting or leaning forward
- Low blood pressure
- Weakness
- Fainting, dizziness, and loss of consciousness
When dealing with cardiac or pericardial tamponade, you’ll come across a collection of three medical signs called Beck’s triad. It is a series of three classic symptoms that will often lead you to suspect cardiac tamponade in a patient.
- Low blood pressure. Blood pressure lowers and the pulse weakens as the force of the fluid in the pericardial sac compresses the heart muscle.
- Jugular venous distension. This is due to the blood having a difficult time returning to the heart that is being squeezed by the fluid surrounding it.
- Muffled heart sounds. The heart tries to compensate for low cardiac output by increasing the heart rate in hopes of increasing the output of blood to systemic circulation. When you auscultate, you will hear muffled heart sounds, as the fluid surrounding the heart will make it difficult to pick up the heartbeat.
Diagnosis and Treatment
To diagnose cardiac tamponade, a full heart examination is required. This includes:
- A physical assessment
- Blood work
- An electrocardiogram to see the electrical activity of the heart
- An echocardiogram to see how blood is flowing and how the heart chambers are functioning
- A thoracic CAT scan to look for fluid in the chest cavity
- An MRI checking the blood flow through the heart
Cardiac tamponade is a medical/surgical emergency. Patients are hospitalized and should be monitored in the intensive care unit.
Supportive therapies such as oxygen and fluid should be given to the patient, and pericardiocentesis should be performed to remove the fluid from the pericardial sac. This procedure involves placing a needle in the pericardial area to drain fluid and might also include cutting a pericardial “window” so fluid will not build up again.
A thoracotomy may also need to be done, depending on the cause of the tamponade, to relieve any fluids from the thoracic area. Once the tamponade is relieved, treating the underlying cause is the next focus of treatment.
If not treated quickly, cardiac tamponade can result in loss of cardiac function and, ultimately, death. Patients with cardiac tamponade should be monitored closely after the procedure to ensure the fluid around the heart subsides completely. In some cases, the fluid buildup can become chronic. But mortality rates are generally low if the condition is quickly diagnosed and treated.
Review Questions
Okay, before we go, let’s go over a couple of review questions to test your knowledge!
1. Warning signs and symptoms of cardiac tamponade are:
- Loud heart sounds
- Chest pain improved by lying supine
- Chest pain made worse by lying supine
- Increased pulse pressure
Chest pain is a prominent symptom and is typically made worse by lying supine and improved by sitting up and leaning forward.
2. Which of the following is NOT a common cause of cardiac tamponade?
- A blunt chest injury
- Acute pericarditis
- A heart attack
- The flu virus
Cases of cardiac tamponade in patients with the influenza virus are very uncommon and are thought to be underreported as incidences are not well known.
That’s all for this review! Thanks for watching, and happy studying!

