Adult ACLS

Welcome to this video on advanced adult cardiac life support, or ACLS, based on the American Heart Association’s algorithms. We will review protocol for responding to cardiac arrest (both non-shockable rhythms and shockable rhythms) and symptomatic bradycardia during this video.
Advanced adult cardiac life support is carried out by medical personnel, such as paramedics, doctors, and nurses, with the appropriate training and access to medications and resuscitation equipment.
Under the cardiac arrest algorithm, the first step is to begin CPR. In some cases, others may already have started CPR, but as the medically trained professional, you should relieve them.
CPR should be administered at 30 compressions to 2 ventilations until an airway is established, compressing to a depth of about 2 inches at a rate of 100 to 120 beats per minute.
If and when an airway is established, oxygen should be administered at a concentration of 100%.
Next, while CPR continues, attach the monitor/defibrillator if it’s not already in place and conduct a rhythm check to determine if the rhythm is shockable or non-shockable. CPR should be paused for no more than 10 seconds to assess the patient’s rhythm.
Shockable and Non-Shockable Rhythms
Shockable rhythms include ventricular fibrillation and pulseless ventricular tachycardia.
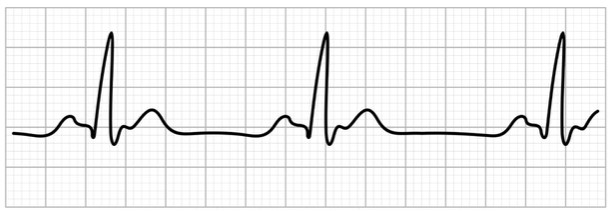
Non-shockable rhythms include asystole and pulseless electrical activity, or PEA. PEA is characterized by a readable rhythm on the monitor, but no palpable peripheral pulse. For this reason, pulse checks should always be done in conjunction with rhythm checks.
Let’s look first at interventions for non-shockable rhythms.
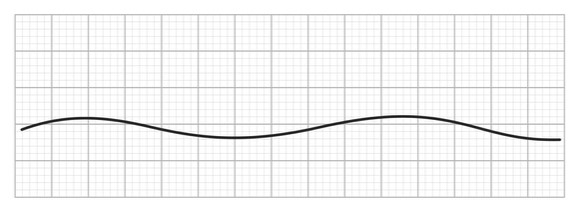
On an electrocardiogram or monitor, asystole is characterized by a flat line, which indicates that both electrical and mechanical activities of the heart have stopped. We sometimes say that a patient has “flatlined.”
With pulseless electrical activity, the tracing will show electrical activity but the mechanical functioning of the heart is not adequate to produce a pulse. This is also referred to as electromechanical dissociation.
Both of these rhythms are considered non-shockable because they indicate that the muscle of the heart is not functioning properly, and therefore would not respond to defibrillation. Once a non-shockable rhythm has been identified, it is critical to administer 1 milligram of epinephrine intravenously or intraosseously as soon as possible, while CPR continues. This may require establishing intravenous or intraosseous access.
You should consider an advanced airway and capnography at this point as well.
Continue to give epinephrine every 3 to 5 minutes if necessary, and alternate 2 minutes of CPR with 10-second rhythm checks because a non-shockable rhythm may convert to a shockable rhythm, or there may be a return of spontaneous circulation (ROSC).
Some important points to remember about resuscitation for asystole or pulseless electrical activity include:
First, change compressors about every 2 minutes or sooner if the individual providing compressions becomes fatigued. Fatigue generally results in insufficient compressions and perfusion may be affected.
Next, take no more than 10 seconds for pulse and rhythm checks every 2 minutes. If the partial pressure of end tidal carbon dioxide is low or decreasing, you must assess the quality of the CPR. Normal pressure is 35 to 40 millimeters of mercury and pressure below 10 millimeters of mercury indicates ineffective compressions. If end tidal carbon dioxide cannot be measured, oxygen saturation via pulse oximetry can be used to assess the quality of CPR.
Intravenous access is preferable to intraosseous for the administration of resuscitation medications, but speed is important, so don’t keep trying for intravenous access if the first attempts fail. The recommended dose of epinephrine is 1 milligram intravenously or intraosseously every 3 to 5 minutes.
Advanced airways may include an endotracheal tube or supraglottic advanced airway. Waveform capnography or capnometry should be used to confirm and monitor endotracheal tube placement. Once an advanced airway is in place, give 1 breath every 6 seconds or 10 breaths per minute without interrupting compressions.
Last, if there is no return of spontaneous circulation, at some point you will need to consider whether to continue resuscitation efforts.
Now, let’s look at interventions for shockable rhythms, which include ventricular fibrillation and pulseless ventricular tachycardia.
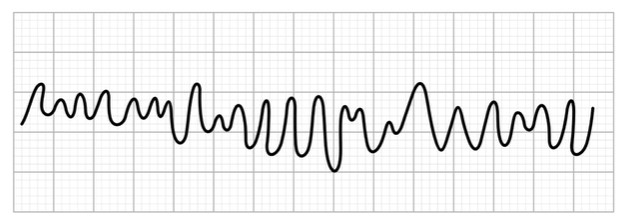
With ventricular fibrillation, the ventricles quiver instead of adequately contracting. This quivering supplies insufficient cardiac output to perfuse the brain and other vital organs, and is very dangerous. The electrocardiogram or monitor tracing is irregular with unformed QRS complexes and an absence of clear P waves.
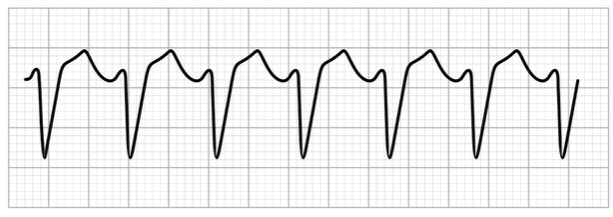
With pulseless ventricular tachycardia, ventricular contractions are very rapid but ineffective because the ventricles are unable to fill adequately, so cardiac output falls. The tracing is characterized by a wide QRS complex and a rate greater than 180 per minute.
Remember that with a non-shockable rhythm, the first thing you do is administer epinephrine because a shock would be ineffective. However, with a shockable rhythm, it’s essential that you administer a shock as soon as the AED or defibrillator is available.
After the shock, immediately resume CPR for 2 minutes and establish an intravenous or intraosseous access. Check the rhythm again after these 2 minutes, and if it remains shockable, give a second shock, and then immediately resume CPR and begin to administer epinephrine every 3 to 5 minutes. An advanced airway and capnography should also be considered at this point.
Check the rhythm again and if a shockable rhythm persists, give a third shock before resuming CPR. At this point, you may administer amiodarone or lidocaine and treat reversible causes.
Reversible causes of cardiac arrest to be considered include the 5 Hs and 5 Ts:
- Hypovolemia
- Hypoxia
- Hydrogen ion (acidosis)
- Hypo or hyperkalemia
- Hypothermia
- Tension pneumothorax
- Cardiac tamponade
- Toxins
- Pulmonary thrombosis AND
- Coronary thrombosis
Some important points to remember about resuscitation for ventricular fibrillation or pulseless ventricular tachycardia include:
First, with a monophasic defibrillator, shocks of 360 joules are delivered. With a biphasic defibrillator, shocks of between 120 and 200 joules are delivered. Next, epinephrine is administered at 1 milligram intravenously or intraosseously every 3 to 5 minutes.
The first dose of amiodarone is a 300 mg bolus intravenously or intraosseously and the second dose is 150 milligrams. Alternatively, lidocaine is administered at a first dose of 1 to 1.5 milligrams per kilogram and a second dose of 0.5 to 0.75 milligrams per kilogram.
CPR and advanced airways are the same as for non-shockable rhythms. Take no more than 10 seconds for pulse and rhythm check every two minutes. If there is no return of spontaneous circulation, you will need to consider whether to continue resuscitation.
Last, if there is a return of spontaneous circulation, then you will continue with post-cardiac arrest care.
Symptomatic Bradycardia
Finally, let’s look at interventions for symptomatic bradycardia, which is characterized by a pulse below 60 beats per minute accompanied by symptoms of inadequate oxygenation. If bradyarrhythmia (a slow and irregular pulse) is present, the rate is usually less than 50 beats per minute.
The symptoms of symptomatic bradycardia may include:
- Chest pain
- Shortness of breath
- Exercise intolerance
- Fatigue
- Syncope (or fainting)
- Impaired cognition or confusion AND
- Dizziness
Please note that bradycardia alone is not pathological. Asymptomatic bradycardia is normal in some individuals, such as athletes and women of small stature.
If a patient presents with bradycardia, the first step is to assess appropriateness for clinical condition; that is, are there symptoms present?
The next step is to identify and treat the underlying cause. Actions include the following:
- Maintain a patent airway and assist with breathing as necessary.
- Provide oxygen if the individual is hypoxic.
- Apply a cardiac monitor to identify and record rhythm, blood pressure, and oximetry
- Apply a 12-lead ECG if available but don’t delay therapy to do so
- Consider possible hypoxic and toxicologic causes.
If the bradyarrhythmia is persistent, consider whether it is accompanied by
- Hypotension
- Acutely altered mental status
- Signs of shock
- Ischemic chest discomfort, OR
- Signs of heart failure.
If the answer is NO, continue to monitor and observe.
If, however, the answer is YES, then treatment is needed.
The first treatment is generally atropine with a first dose of a 1 milligram bolus, repeated every 3 to 5 minutes to a maximum of 3 milligrams.
If the atropine in ineffective, then treatment may include
- Transcutaneous pacing AND/OR
- a dopamine infusion OR
- an epinephrine infusion.
If symptoms persist, consider expert consultation and transvenous pacing.
When administering dopamine, it is given intravenously at 5 to 20 micrograms per kilogram per minute, titrated to the patient’s response, and then slowly tapered to the patient’s tolerance.
Epinephrine is given intravenously at 2 to 10 micrograms per minute and titrated to patient response.
Some of the causes of persistent bradyarrhythmia include:
- Myocardial ischemia or infarction
- Toxicologic drugs, such as calcium channel blockers, beta blockers, and digoxin
- Hypoxia, AND
- Electrolyte abnormalities, most commonly hyperkalemia
Remember that time is the critical element in the care of a patient in cardiac arrest or experiencing symptomatic bradycardia.
The longer it takes before treatment is administered, the more likely that the patient will develop neurological deficits or die.
That’s all for this review! Thanks for watching, and happy studying!
