Jaundice Icterus

Welcome to this video review on newborn jaundice, also known as icterus or hyperbilirubinemia. About 50-60% of all newborns have jaundice in the first week of life, and if often goes away. However, there are times when bilirubin levels get too high and must be treated to prevent further problems. In this video we will look at what jaundice is, what causes it, risk factors, signs, diagnosis, and treatment.
Jaundice happens when bilirubin builds up in the baby’s blood, causing the skin and whites of the eyes to look yellow. Bilirubin is an orange-yellow pigment that is a waste product.
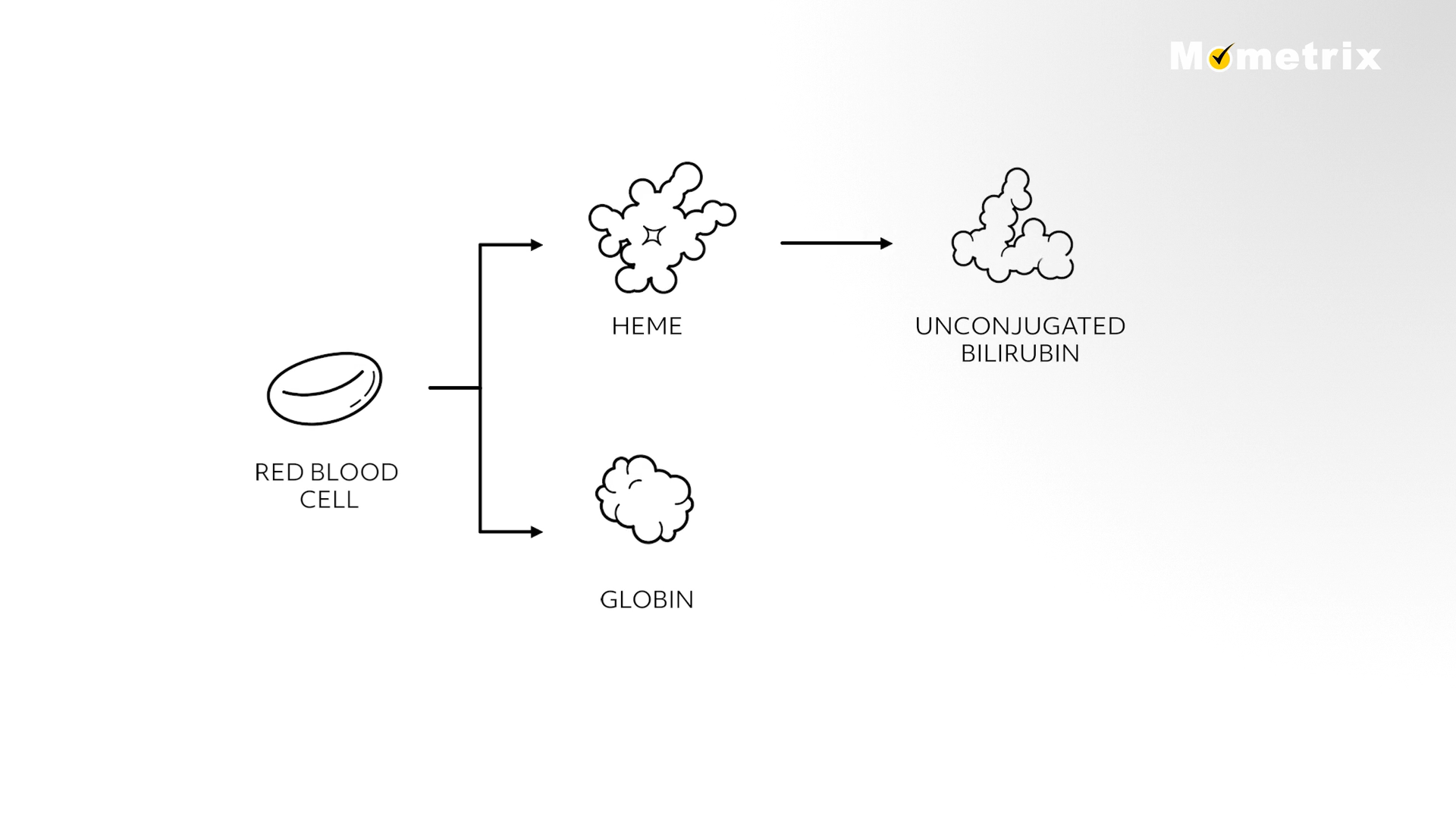
When red blood cells are broken down, they are broken up into HEME and GLOBIN, of which the HEME is further broken down into unconjugated bilirubin. The unconjugated bilirubin is lipid-soluble (therefore not water-soluble) and binds to albumin, then travels to the liver and becomes water-soluble through the process called conjugation. Conjugated bilirubin is excreted into the GI tract through the bile duct and leaves the body through newborn stool. During pregnancy, the mother’s liver is removing bilirubin for the baby, but after birth the baby’s liver must remove the bilirubin and sometimes the liver is not developed enough to get rid of the bilirubin.
Physiologic hyperbilirubinemia occurs in almost all neonates, with bilirubin levels at their highest by 3 to 4 days of life, then decreasing thereafter. This increased bilirubin production occurs because RBCs (red blood cells) are breaking down fast, which results in increased bilirubin production. Also, the newborn’s liver is immature and cannot conjugate the bilirubin to remove it from the body efficiently. Breastfeeding jaundice may occur in the first week of life in newborns who do not consume enough breast milk. These babies have fewer bowel movements, and therefore eliminate less bilirubin. Encourage mothers to increase breastfeeding and as infants consume more, the jaundice disappears on its own. Breast milk jaundice syndrome is different from breastfeeding jaundice in that it is caused by an abnormality in the breast milk that interferes with the liver getting rid of bilirubin from the body. It occurs at one to two weeks of age and may persist for several months. It generally needs no therapy if the serum bilirubin remains below 15 mg/dL in healthy full-term infants. If it rises above 15 mg/dL, temporary interruption of breastfeeding for 1-2 days may be needed. Pathologic hyperbilirubinemia is due to an excessive breakdown of RBCs that overwhelm the newborn’s liver with more bilirubin than it can process. This can be caused by an immune disorder or nonimmune disorder. Immune disorders cause destruction of RBCs when the fetus’s blood type is incompatible with the mother’s – the mother’s blood is Rh-negative and the fetus has Rh-positive blood. This problem can be prevented by giving the mother injections of Rh antibodies. Nonimmune causes of excessive RBC breakdown include hereditary RBC disorders or bruising that occurred during birth. The breakdown of blood from a large hematoma (bruise) may cause jaundice.
Risk Factors
There are some infants that have risk factors leading to higher bilirubin levels and severe jaundice. Preterm infants, those born before 37 weeks, do not have a fully developed liver and may not be able to get rid of the bilirubin adequately. Infants that have a sibling that had jaundice or infants that are of East Asian or Mediterranean descent are at higher risk of developing jaundice. An infant that is not eating well, and not voiding and stooling well in the first days of life may develop an increased bilirubin level. Bruising at birth causes high levels of bilirubin and mothers with type O or Rh negative blood tend to have infants with higher bilirubin levels.
Diagnosis
Neonatal jaundice is usually first seen as a yellowish discoloration of the face, then the chest, moving to the abdomen, arms, and legs as bilirubin levels increase. The whites of the eyes may also appear yellow. Gently press on the baby’s skin with a finger and look to see if the skin is yellow before the pink color returns. If jaundice is suspected in a newborn, the mother’s medical history should be evaluated for TORCH infections, maternal diabetes (which can cause early hyperbilirubinemia), Rh incompatibility, prolonged or difficult birth (causing a hematoma or forceps trauma to infant). It is also helpful to know if any siblings of the newborn had jaundice. Particular areas of concern include jaundice on the first day of life; jaundice after 2 weeks of age; lethargy, irritability, respiratory distress; total serum bilirubin (TSB) > 18 mg/dL or TSB increasing > 5 mg/dL/day. ….Bilirubin levels can be tested noninvasively with a transcutaneous (TC) measurement on the sternum. TC bilirubin has been shown to correlate with serum bilirubin measurements, and should be checked on all infants at 24 hours of age, or earlier if positive signs are present. If the TC bilirubin is elevated, serum bilirubin levels should be tested also by doing a heel stick blood draw. …A bilirubin > 10 mg/dL in preterm infants or > 18 mg/dL in term infants is reason for additional testing, including total and direct serum bilirubin, Hct, direct Coombs test, reticulocyte count, blood smear, and blood type of infant. For newborns > or equal to 35 week gestation, risk of hyperbilirubinemia is based on a graph of the newborn’s age in hours and the TSB level.
A major consequence of neonatal hyperbilirubinemia is neurotoxicity. Unconjugated bilirubin is lipid-soluble, can cross the blood-brain barrier and be deposited in the brain, causing neurologic deficits, including cerebral palsy and sensorimotor deficits. The most severe form of neurotoxicity is kernicterus, which causes hearing loss, irreversible brain damage, and/or death.
Treatment
Phototherapy is the standard treatment and uses a fluorescent white light or blue light to conjugate the free bilirubin and increase its secretion. For a term infant, phototherapy is an option when unconjugated bilirubin is > 12 mg/dL at 24 hours of life, > 15 mg/dL on 2nd day of life, and > 18 mg/dL on 3rd day of life. If the infant is preterm, the bilirubin levels for treatment are lower because preterm infants are at greater risk of neurotoxicity. When an infant is under phototherapy, the eyes and genitals should be covered to protect from the light. Serum bilirubin levels should be checked regularly to evaluate the effectiveness of phototherapy. Also, lights should be turned off when blood is drawn, because bilirubin in the collection tubes may rapidly photo-oxidize. If hyperbilirubinemia is severe, exchange transfusion may be necessary. This involves rapidly removing bilirubin from circulation by withdrawing small amounts of blood and replacing it with donor Red blood cells. There are risks and complications involved with the procedure, but the success of phototherapy has reduced the need for frequent exchange transfusions.
Let’s review a couple of questions:
Review Questions
The postpartum nurse is giving instructions to the mother of a breastfed infant with hyperbilirubinemia. Which instructions are the most appropriate to give the mother?
- Feed the infant less frequently and return to doctor’s office in 1 week to have bilirubin rechecked.
- Stop breastfeeding and switch to bottle-feeding permanently.
- Continue to breastfeed at least every 2-3 hours, watch for 2 to 5 bowel movements every 24 hours, and follow up with the doctor in 2 to 3 days to have the bilirubin rechecked.
- Switch to bottle feeding the infant for 2 weeks, and use a breast pump to maintain milk supply.
It is most appropriate to increase breastfeeding, which increases elimination of bilirubin through bowel movements.
Let’s try another one…
The dangers of untreated newborn jaundice include
- Icterus
- Kernicterus
- Neurologic deficits
- Both B and C
A major consequence of neonatal hyperbilirubinemia is neurotoxicity, causing neurologic deficits, the most severe form being kernicterus, which causes hearing loss, irreversible brain damage, and/or death.
Thank you for watching this video tutorial on newborn jaundice! Be sure to check out our other videos!
